Laparoscopy is a diagnostic or surgical intervention on the internal organs of the abdominal cavity or pelvis. Laparoscopy is a modern surgical method in which surgery is performed not through natural openings or large skin incisions, but through small (usually 0.5-1.5 cm) punctures, whereas conventional surgery requires large incisions and thus leaves large scars. For puncture, a trocar is used, with the help of which the abdominal wall is pierced, and a thin optical device (laparoscope) is inserted into a tube with a diameter of 0.2-1.0 cm.
The main tool for laparoscopy is the laparoscope – a metal tube with a diameter of 5-10 mm (2 mm for micro laparoscopy) with a complex lens system and light guide. The lens transmits the image from the lens to the eyepiece, and the light guide directs the light beam from the illuminator into the abdominal cavity. You can look directly into the laparoscopic lens – this has been done for decades, but with the advent of tiny endoscopic cameras (now they weigh 50-150 grams) attached to the laparoscopic lens in the last three decades, all operating room personnel can see all the progress of the operation on the monitor. Diagnosis and some simple procedures are performed under local anesthesia, and most laparoscopic procedures are performed under general anesthesia.
There is no such thing as “laparoscopic surgery”. Laparoscopy is one of the methods of accessing surgical organs. Regardless of the method of implementation, the nature of the surgical procedure does not change. These terms are formed using the root word “scope” (from the Greek scope-I see), the first half of the method’s name denoting the organ or cavity being manipulated or examined.
Laparoscopy is one of the varieties of endoscopy, and endoscopy includes laparoscopy, thoracoscopic examination, hysteroscopy, cystoscopy, arthroscopy and so on.
Thoracoscopy – intervention on the chest;
Nephroscopy – intervention and surgery on the kidneys;
Cystoscopy – surgery on the bladder;
Hysteroscopy – surgical intervention on the uterus;
Gastroscopy – surgery on the stomach.
If the prefix “fibro” is added to the name, it means that the procedure is performed using a flexible endoscope, for example, fiber hysteroscopy is an examination of the uterus using a flexible endoscope.
The technique of laparoscopic surgery varies slightly depending on the type of surgery and the medical institution. Patients are prepared to receive the same care as conventional surgery. First, the patients in the ward are injected with drugs for further pain relief and enhanced efficacy. These operations are called “preoperative administration”. The patient is then carried to the operating room on a stretcher.
A soft plastic catheter is inserted into the patient’s cubital vein for infusion of medicines, solutions, anesthetics, and pain relievers. A rubber or silicone mask is attached to the patient’s face and the breathing mixture is supplied through the mask.
Seconds later, the patient falls asleep and the anesthesiologist intubates — he inserts a cuffed plastic tube into the airway, inflates and secures the airway. During surgery, the patient receives controlled artificial lung ventilation.
For laparoscopy, the abdominal cavity is filled with gas – in most cases, carbon dioxide is used for this purpose. Gas is injected to elevate the abdominal wall to a dome shape above the organs and provide good visibility and access to the organs. Assistants and surgeons treated the patient’s entire abdomen with antiseptic solutions for a possible transition to open surgery and, at the anesthesiologist’s orders, inserted a long Veress needle through the navel. It is designed with a spring-loaded core to minimize possible damage to the underlying internal organs during abdominal puncture. After confirming with the help of several tests that the needle is indeed in the abdominal cavity, the hose of the insufflator is attached to the needle. This sophisticated electronics allows supplying carbon dioxide into the cavity and automatically maintains the pressure therein with an accuracy of 1 mmHg.
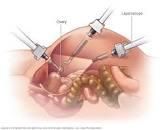
After the gas pressure in the cavity reaches 10-16 mmHg (depending on the surgeon’s choice), the Veress needle is removed and the first trocar is inserted through the navel – a metal or plastic tube into which a trihedral or tapered probe is inserted. After puncturing the wall, the stylet is removed and inserted through the cannula (tube) into the endoscope and laparoscope. A laparoscope is a 10, 5 or 2 mm diameter (using a micro laparoscope) metal tube with a complex lens system and light guide. With attached miniature video cameras weighing 50-100 grams and powerful halogen or xenon light sources (illuminators), the entire operating team can observe the progress of the operation on a monitor screen.
After introducing the laparoscope, inspect the abdominal cavity and insert 2-4 more trocars under visual control. The point of trocar introduction depends on the organ being operated on and the type of intervention – in cholecystectomy, the trocar is inserted in the upper abdomen below the costal arch, in gynecological surgery – in the lower abdomen.
In principle, instruments with a length of 30-40 cm and a diameter of 2 to 12 mm can perform all the same operations as conventional surgical techniques. Retention, abduction to the side, capture of the organ with clips, release and separation of the organ from surrounding tissue (dissection) by means of dissectors, endoscopic scissors and electrosurgical instruments, with the help of coagulation, relative cessation of bleeding small vessels. Coagulation – proteins fold under the influence of high-frequency alternating current, so the lumen of the blood vessel closes. Bleeding from large vessels can be stopped by clipping (using titanium clips), banding with suture material, and suturing with an endoscopic stapler
Endoscopic staplers play a very important role in endoscopic surgery – this may seem unusual, but instead of a scalpel the surgeon is holding a needle holder for much longer – The process of stitching, suturing, and bandaging takes much more time than tissue dissection. A skilled surgeon can tie approximately 60 safety knots per minute, or one knot per second. Meanwhile, in endoscopic surgery, the surgeon’s hands are replaced by slender instruments that are much more difficult to tie. So, for example, the European Association of Physicians and Surgeons set a standard – tie a triple knot in 40 seconds. So this was a revolutionary innovation that played a very important role in expanding the scope of endoscopic interventions, the staplers. Surgeons can perform inter enteric anastomoses with one motion of the hand, sealingly pass through the intestine, suture bleeding vessels, etc., instead of the long and sometimes almost impossible manual endoscopic suturing. It has become technically possible to perform any surgical operation by endoscopic surgical approach with the help of a stapler.